By Jacqueline Tempera
The Providence Journal, R.I.
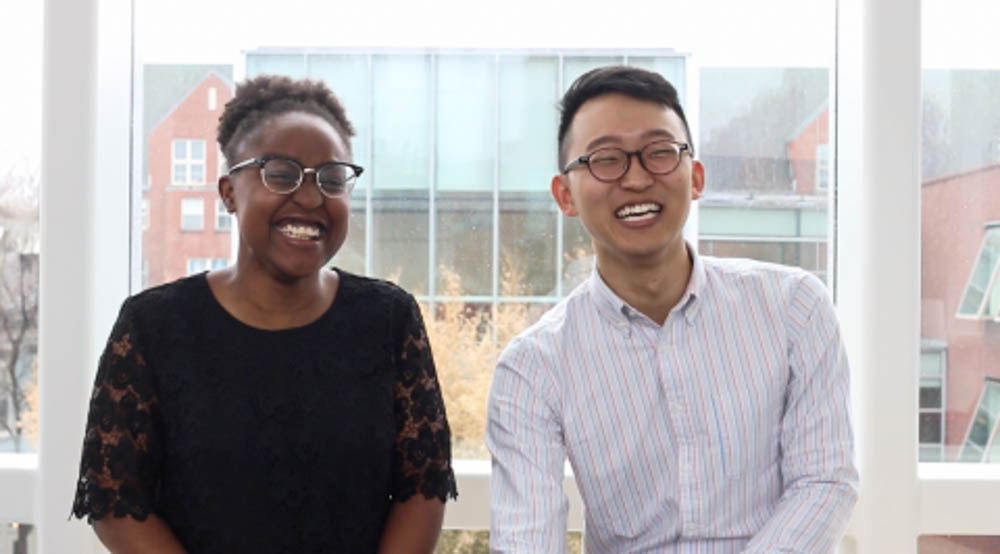
WWR Article Summary (tl;dr) Brown students Richard Park and Bella Okiddy said they wanted to find a way to apply their biomedical engineering degrees to improve rape kits. With their new venture “Technologies Against Assault,” Okiddy and Park, both 23, have developed technology for color-changing cotton swabs that would activate if they came in contact with semen.
PROVIDENCE, R.I.
What if collecting forensic evidence after a sexual assault was as simple as taking an at-home pregnancy test? Brown University students Richard Park, a graduating senior, and Bella Okiddy, a graduating master’s student, say it can be.
With their new venture “Technologies Against Assault,” Okiddy and Park, both 23, have developed technology for color-changing cotton swabs that would activate if they came in contact with semen. This is an invention, which would cost about 20 cents more per swab, that would be “transformative for the field,” says Heather Aliotta, a sexual-assault nurse examiner at Women & Infants Hospital.
Park and Okiddy said they wanted to find a way to apply their biomedical engineering degrees to improve rape kits. Park, who is from Atlanta, draws on his own experience. When he was 18 and visiting prospective colleges, he was sexually assaulted by another man during a night of heavy drinking. He never reported it, he said.
“It’s something that’s always in the back of my mind,” he said. “I want to empower survivors to seek medical attention, not just for [sexually transmitted infections], or potential pregnancies. But also, as the first step in a healing process. I never had that.”
After a sexual assault, the clock starts ticking, said Aliotta, a Brown alumna who has been advising Okiddy and Park. At maximum, a victim has 96 hours to reach a hospital and collect DNA evidence for prosecution.
And even then “unless she was curled up in fetal position, hasn’t left her house, showered, bathed or changed clothes,” since the assault, “the potential for good, usable evidence is very low,” Aliotta said.
The last step of a “rape kit” exam is the collection of biological evidence. It’s invasive, and can take hours, Aliotta said.
The examiner must swab each suspected penetration area multiple times to “maximize evidence collection,” she said.
Then, it’s a waiting game. In many states it can take months, or years, to receive results, according to End The Backlog, a Joyful Heart Foundation program that seeks to provide information about untested rape kits in the United States.
In Rhode Island, a victim generally receives results in one month, according to Joseph Wendelken, a spokesperson for the state Department of Health. With Park and Okiddy’s innovation, it could be reduced to minutes.
“One of the hardest things is dealing with a patient that can’t remember what happened, whether it’s because of drugs, drinking or trauma,” Aliotta said. “This technology would hopefully give some answers a lot sooner. Patients would have some validation and closure leaving the hospital.”
Its use would also be limited to the “most common image of rape,” Aliotta said, which is “penile, vaginal rape with ejaculation.” It could confirm the existence of sperm, as with an at home pregnancy test; additional tests would be required for certainty or specific DNA matching.
Park and Okiddy said they came up with the concept while drinking tea and “ideating” — their distinctly Ivy League word for brainstorming. It wasn’t until Park mentioned it to his scientific adviser, Anubhav Tripathi, that they realized they had something good.
Tripathi has been guiding the pair’s research. He is also lending his expertise in microfluidics to help them work on expediting the forensic testing process, which is a secondary part of their project.
Park and Okiddy recently won the Swearer Center for Public Service’s Embark Postgraduate Fellowship, which will match funds they raise through their crowdfunding campaign on Indiegogo.com, giving them about $50,000 in total to buy samples and begin product development.
By December 2017, they hope to get U.S. Food and Drug Administration approval, Park said. The Rhode Island Center for Forensic Sciences, which purchases all rape kits for the state, and the Sexual Assault Nurse Examiner team at Women & Infants Hospital have expressed interest in the product.
Each young scientist has a distinct goal. For Okiddy, it’s bringing the technology back to her native Kenya. Park hopes to create an environment here in the U.S. where victims aren’t afraid to seek medical attention after an assault.
Park’s assault, and the support of other victims, have kept the pair motivated, said Okiddy.
“That’s become our fuel,” she said. “It’s thanks to the people who have stepped forward and shared their stories in support of our idea when they didn’t have to.”
That in itself, Park said, is “enough motivation to last more than one lifetime.”
For more information or to donate, search “Technologies Against Assault” on Indiegogo.com.
Nationally, there are 144,407 untested rape kits
Nationally, there are at least 144,407 untested rape kits, according to data compiled by End the Backlog. This number does not include figures from 20 states, including Rhode Island, that have not provided an accurate count.
U.S. Senate Bill 2063, introduced in January, would require every state law enforcement agency to compile a report of the number of untested kits in their possession by Feb. 1, 2017. It’s under review by the Senate Judiciary Committee.
What is a “rape kit”?
A sexual-assault evidence collection kit, or a rape kit, is a package that includes bags and paper sheets for evidence collection, a comb, documentation forms, envelopes, instructions, swabs, and materials for blood samples.
The exam has multiple steps including:
— Listen to victim’s recollection of the incident
– — Collect clothes
— Photograph injuries
— Gather of biological evidence (by cotton swabbing mouth, vagina, rectal area, skin and collecting hair combings, pubic hair combings, and under the nail tissue)