By Sandra G. Boodman
Kaiser Health News
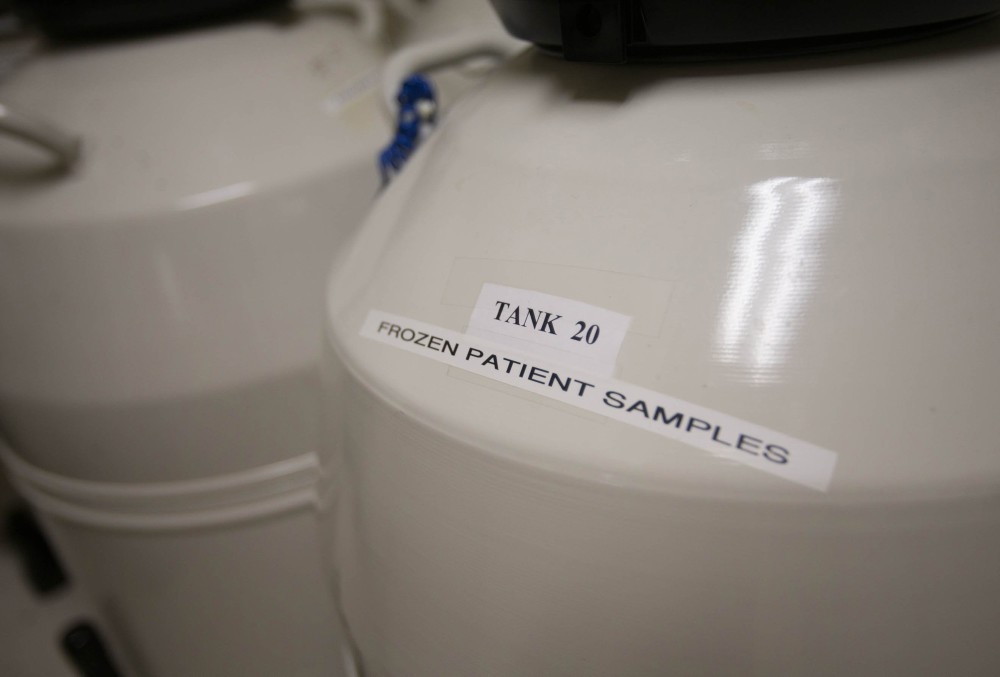
WWR Article Summary (tl;dr) Fertility specialists say that egg donation is safe and involves the same process as in vitro fertilization, which uses drugs to stimulate and regulate egg production. However, studies of the long-term impact of egg donation on donors have never been done, even though the practice dates back more than 30 years.
Kaiser Health News
Maggie Eastman considers it the worst decision she ever made.
In 2003, beset by $30,000 in tuition debt and imbued with a burst of altruism, Eastman, a college senior, decided to donate her eggs to help an infertile couple have a baby. Over the next decade she donated nine more times, earning a total of about $20,000, money that helped Eastman and her then-husband buy a house.
“When I think back, I think, ‘God, how stupid was I?'” said Eastman, now 34, who works as a 911 operator near Seattle. She made her final donation in 2013, months before she was diagnosed with Stage 4 metastatic breast cancer, a rarity in someone so young who has no family history of the disease.
Eastman said that when she asked her oncologist whether her cancer might be related to her egg donation, which involves the use of hormones to rev up egg production, he replied that he didn’t know, adding, “Well, there are risks.”
Although Eastman believes that being an egg donor was the cause of her estrogen-fueled cancer, experts say it is impossible to know. Studies of the long-term impact of egg donation on donors have never been done, even though the practice dates back more than 30 years.
Despite sporadic reports of subsequent infertility and a variety of cancers, some fatal, it isn’t known whether these problems are linked to the process or are simply the result of chance.
Fertility specialists say that egg donation is safe and involves the same process as in vitro fertilization, which uses drugs to stimulate and regulate egg production. A 2013 meta-analysis of 25 studies seeking to evaluate the risks between ovarian cancer and the use of fertility drugs found “no convincing evidence” of an increase in the risk of invasive ovarian cancer.
“There are no long-term adverse risks of IVF” or egg donation, said Richard J. Paulson, president-elect of the American Society for Reproductive Medicine (ASRM), which represents fertility specialists. Paulson heads the infertility program at the University of Southern California, one of the nation’s oldest egg donor programs, which was established in 1986. “All the data we have so far seem to indicate no long-term problems.”
But others say the matter remains unsettled because donors haven’t been studied.
“There is a total lack of information about the long-term (effects),” said Timothy R.B. Johnson, the longtime chairman of the department of obstetrics and gynecology at the University of Michigan Medical School.
Johnson supports the establishment of a national registry to track the health of egg donors. “No one’s collecting the data” on donors, he said, adding that the fertility industry is largely unregulated. Once their eggs are retrieved, donors are sent home with little or no follow-up.
A transaction once shrouded in secrecy, the internet now hosts a thriving and competitive marketplace for donors, largely supplanting leaflets on college bulletin boards and ads in campus newspapers, the traditional methods of recruiting fertile young women. Payment varies, currently starting at about $3,500 per cycle and sometimes exceeding $50,000, depending on the location of the clinic or egg brokerage and the donor’s characteristics. An Ivy League education, Asian descent (there is a paucity of donors), exceptional looks and a previous donation that led to a birth command higher reimbursement.
The demand for donor eggs has increased rapidly in the past decade. Nearly every state has at least one fertility clinic, said Judith Daar, a specialist in reproductive law and a professor at Whittier Law School in Costa Mesa, California. A report in JAMA found a significant increase in the use of donor eggs between 2000 and 2010, from 10,801 to 18,306. Daar estimates that about 10,000 babies born in the United States in 2013 were conceived using donor eggs.
But questions about egg donation abound, said veteran women’s health advocate Judy Norsigian, a co-founder and former executive director of the Boston-based advocacy group Our Bodies Ourselves. Among the unknowns: How many women have donated eggs? (The number is believed to be in the thousands.) How many times are they donating? (The ASRM recommends a lifetime maximum of six.)
Which drugs are they being given, and in what doses? How common is ovarian hyperstimulation syndrome, a painful condition in which the ovaries swell? Severe cases can lead to a stroke or even, rarely, to death.
___
It is also difficult, health advocates say, to gauge how aware potential donors are, or what they are told, about short- and long-term risks.
A 2010 study of 80 donors found that “a rather large and troubling minority”, 20 percent, said they did not know of possible health risks. And while 8.8 percent said they knew that the process entailed some pain, 45 percent reported experiencing “notable pain.” A 2014 study of egg donation ads placed on Craigslist, one of the chief venues for egg donors, found that “the vast majority” do not include risk information.
Norsigian said she worries that donors are being falsely reassured that the process is safe, without being told that there is no definitive research.
“Absence of evidence of harm is not proof of safety,” she said. “Fertility doctors by and large don’t want to shine a light on what is a really lucrative field.”
Studies of IVF in infertile women have produced conflicting results: Some have found no increase in cancer, while others reported an increased risk of uterine and ovarian cancer. The meaning of this finding is unclear, because infertility itself is a risk factor for some malignancies.
Some fertility specialists are cool to the idea of a registry, which they say is unnecessary. “I can’t even imagine logistically that such a thing would ever take place,” said Preston Sacks, a reproductive endocrinologist affiliated with Columbia Fertility Associates, which has three offices in the Washington, D.C., area. In Sacks’ view, concerns about medical privacy would prove insurmountable.
Judy E. Stern, a professor of pathology and obstetrics and gynecology at Dartmouth who oversees the Infertility Family Research Registry, a voluntary database that includes about 70 egg donors, said she believes that donor data is urgently needed.
“I think if there had been huge health risks (from IVF), we would have seen that over the last 30 years,” she said. “That suggests the absolute risk is fairly low. But we don’t know anything about the donors,” whose risks may differ from infertile women undergoing IVF. “These are presumably fertile women and they may respond to medications (differently) than infertile women.”
Stern co-chairs an egg donor task force of the Society for Assisted Reproductive Technology, which represents clinics performing IVF. She said SART is considering the establishment of an egg donor registry. “If we don’t understand the risks for donors, we need to, because of the women who are freezing their eggs” for possible later use, she said.
___
Ari Laurel, now 26, donated her eggs to an Australian couple in 2014. Laurel said that she knew she didn’t want children and that Asian donors like her were in demand. Her $12,000 payment financed a year of graduate school. “The agency I went through seemed to ask eugenic-type questions” such as skin color and whether she had been in gifted programs. Laurel said she was also asked to submit her undergraduate transcript and GRE scores.
Laurel, who lives in Missoula, Mont., said she felt well informed by the clinic about possible health risks and suffered no complications. Before deciding to donate, she contacted We Are Egg Donors, an online group founded in 2013, and spoke to one of its founders.
She has no regrets and is happy that she was able to help an infertile couple have a baby. But when the clinic contacted her for a second donation, Laurel declined. “I found the process pretty exploitative,” she said.
Her savvy is not typical of the 60 egg donors whom medical anthropologist Diane Tober has interviewed for a film she is making. Tober, an assistant professor of nursing at the University of California, San Francisco, said that some donors seemed naive about the process, which many found more physically and emotionally daunting than they anticipated.
“They expected that the doctor and the staff was going to look out for them as they do for their infertility patients,” Tober said. The pitch was “cloaked in this language of ‘Be an angel, help someone and get paid for it.'”
Some donors, she said, were motivated by altruism; others said “it would be so cool” to help gay men create a family.
In Tober’s view, egg donation more closely resembles kidney donation than sperm donation. Both egg and kidney donation, she said, “involve drugs and medical procedures that are of no benefit to the donor.”
Sacks, the Washington fertility specialist, said that about 10 percent of the prospective donors he evaluates decide against completing the process once he tells them what’s involved. Donors are paid $8,000 per cycle, he said, and have included a teacher, a lawyer with a major Washington firm and a school bus driver; few are college students.
After undergoing medical and psychological screening and being matched with a recipient, the donor takes birth control pills to synchronize her menstrual cycle with that of the recipient. After that, she typically injects Lupron, a hormone approved to treat advanced prostate cancer. Lupron, which prevents the ovaries from releasing an egg, is not approved for use in fertility procedures. Some women’s health advocates say they are concerned that donors are not told the drug is being used “off label” for an unapproved use. (Off-label use of drugs is common in all fields of medicine.) Lupron’s side effects have aroused concern; they include joint pain, acne and osteoporosis.
Lupron is followed by injections that stimulate egg production. After that comes a carefully timed “trigger shot” of a hormone that causes ovulation. Within roughly 48 hours, the donor is sedated and a needle is inserted transvaginally into the ovary to extract each egg. Typically no more than 20 eggs are harvested.
___
Clinical psychologist Andrea Mechanick Braverman, who screens donors for several Philadelphia area fertility clinics, said that one of her goals is to ensure that donors “know what they’re doing.” She worries that some underestimate the invasiveness of the procedures and the long-term emotional ramifications, such as feelings of regret. “You try to get them to think it through.”
Sindy Wei, 39, thought she had. Wei, an assistant professor of radiology at UCLA, donated her eggs in September 2001; she was then a 25-year-old M.D.-Ph.D. student struggling to pay her rent in Los Angeles.
Wei, who has testified about her experience before a California Senate committee seeking greater protection for egg donors, said she researched the potential risks and found none.
“I didn’t know the research hadn’t been done because the donors hadn’t been followed,” Wei said. A San Francisco clinic paid her $6,500, she said, and extracted a whopping 60 eggs.
When Wei complained in the recovery room that she felt ill, she said doctors tried to discharge her and urged her to fly home to Southern California. Wei said she refused to leave, and eight hours later she was admitted to a hospital after her blood pressure plummeted because she was bleeding out. Doctors discovered that Wei’s ovarian artery had been nicked during the retrieval process and her abdomen had filled with blood. She received several transfusions and underwent emergency surgery, then spent several days in intensive care.
Wei was left with bladder spasms and infertility and underwent six rounds of fertility treatment when she was trying to get pregnant. She said her biggest fear is that she will develop cancer from the hormones she took as a donor and infertility patient.
“I think egg donation should be a choice for young women,” Wei said. “But they should really know what the risks are. And unless it’s studied, there’s no way to tell.”
___
(Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation.)