By Angie Leventis Lourgos
Chicago Tribune
WWR Article Summary (tl;dr) As Angie Leventis Lourgos reports, these cases “provided early insight into everything from how the virus sheds to the length of time a patient is contagious to how COVID-19 is transmitted.”
Chicago
She was known as Patient 1.
The Chicago woman in her 60s had traveled on Christmas Day to Wuhan, China, where she cared for her elderly father who had fallen ill to a mysterious, undiagnosed respiratory sickness.
After returning to Chicago in mid-January, her own symptoms emerged: fever, cough and fatigue, followed by nausea and dizziness.
While hospitalized for pneumonia, she became the first patient in Illinois and the second in the nation to test positive for the novel coronavirus, a new and little-understood illness that would soon burgeon into an international pandemic, sickening millions and altering all aspects of daily life across the globe.
Her husband, who had not gone to China, also tested positive days later, marking the first documented case of person-to-person transmission in the United States.
What medical experts learned from that local couple, through lengthy interviews, rigorous coronavirus testing and analysis of so many of their specimens, helped shape much of the nation’s earliest knowledge of the virus, which would later be called COVID-19.
The wife and husband remained anonymous to the public even after their recovery and discharge to home isolation in early February. Hospital officials said the wife in particular feared ostracism at a time when bigotry and xenophobia stemming from the virus hit a fever-pitch here and around the world.
“Please do not let fear or panic guide your actions,” a leader with the U.S. Centers for Disease Control and Prevention implored the nation in late January. “For example, please do not assume that just because someone is of Asian descent that they have this new coronavirus.”
Rhetoric on many social media platforms had blamed the first Illinois patient for bringing the virus to the Chicago area.
“Send her back,” one local man had posted on Facebook when news broke of the first confirmed case.
“To (sic) many people coming here from other countries bringing in disease,” a woman wrote on the site. “Keep out!”
Scientists now know the highly contagious virus, which has since infected nearly every country, leaving few parts of the world unscathed, was already spreading undetected across the U.S., possibly as early as December. The Chicago couple were simply among the first to be diagnosed.
Yet their bodies and oral testimony provided early insight into everything from how the virus sheds to the length of time a patient is contagious to how COVID-19 is transmitted. These first cases also helped health officials develop infection control protocols, testing guidelines and best use of personal protective gear for staff, as well as the earliest local coronavirus contact tracing operation.
The wife and husband were treated in isolation at Amita Health St. Alexius Medical Center Hoffman Estates, a midsize northwest suburban hospital that suddenly found itself in the epicenter of scientific inquiry and research into a world health epidemic.
Field teams from the CDC quickly converged with state, county and local health leaders, forming a makeshift command post of sorts in the basement of the hospital. To help draft a road map for care, hospital administrators contacted officials at the hospital in Washington state where the first U.S. coronavirus case had been confirmed days earlier.
New information was constant, and constantly changing, recalled Polly Davenport, president of St. Alexius.
“Guidelines, protocols, testing,” she said. “Just a lot of information coming very rapidly. Our team did a great job. But I’ve been through hurricanes, I’ve been through power outages. This was a lot of unfamiliar information coming very quickly.”
The CDC announced on Feb. 25 that the new coronavirus “will almost certainly spread in the United States,” and urged schools, health facilities and businesses to prepare.
In retrospect, some local medical experts credit the state’s early and aggressive COVID-19 precautions to these first two Illinois patients, who served as a harbinger of what was to come.
“It was almost a double-edged sword to have gotten the second case in the United States, because it was pretty taxing on our agencies,” said Dr. Kiran Joshi, senior medical officer and co-lead of the Cook County Department of Public Health. “But at the same time, we were forewarned in a way of what could happen, and I think as a whole reacted much more quickly than perhaps other states.”
Gov. J.B. Pritzker issued an executive statewide stay-at-home order that began March 21, one of the earlier and more stringent government-mandated policies of its kind at the time. These restrictions were eased starting at the end of May, later than many other parts of the country.
While these measures faced much criticism and multiple legal challenges, the governor pointed to declining COVID-19 positivity rates and deaths as metrics indicating early success. Even as the pandemic reached its peak here in May _ and with 30 counties currently at a “warning level” for resurgence _ Illinois has never lacked hospital beds or ventilators.
“While we definitely had a surge, there was never a point where our hospitals were overwhelmed,” Joshi said. “We put into place the appropriate public health measures statewide to prevent that.”
The first Illinois patient tested positive for the coronavirus on Jan. 23, back when the virus still felt thousands of miles away, mainly afflicting China.
This was before social distancing became standard practice in the U.S. Before in-person school felt like a weighty decision. Before masks were required and routinely worn in most public spaces. Before the World Health Organization on March 11 declared COVID-19 a worldwide pandemic.
“It feels like it was years and years ago, because the time between then and now has been so full with COVID and the pandemic in the United States,” said Dr. Rachel Rubin, senior medical officer and co-lead of the Cook County Department of Public Health.
Joshi recalled meeting Patient 1 the day after she tested positive.
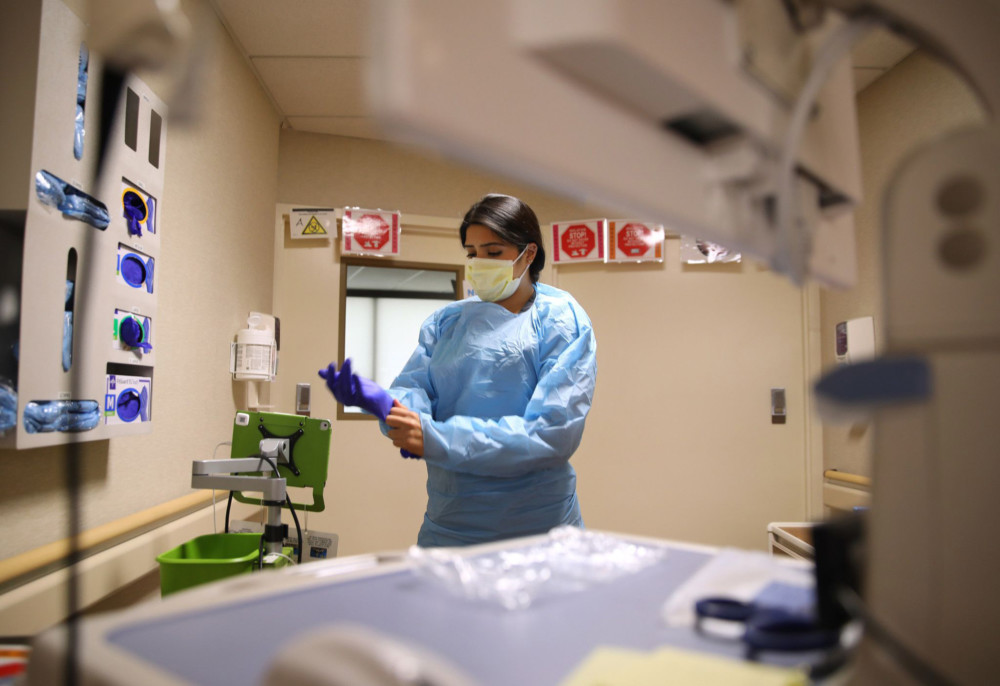
Before entering her negative air pressure room at St. Alexius, he and a colleague from the CDC both donned full personal protective equipment, disposable gloves, gowns, eye protection and N95 masks.
It was a tense moment. So little was known about the new coronavirus, but both health officials had seen news coverage of so many deaths linked to the virus in China.
“We made eye contact in our PPE, and we just shrugged and walked in,” Joshi said. “Like, here we go.”
On Jan. 30, the first patient’s husband tested positive as well. He already suffered from chronic obstructive pulmonary disease, causing a cough and labored breathing, so it wasn’t clear at first that his symptoms stemmed from COVID-19, according to an article published in the medical journal The Lancet in April.
Joshi described both the wife and husband as very forthcoming, giving multiple interviews that lasted hours, rehashing details of what they experienced and any possible contact they might have had with others post-infection.
Health officials from the hospital and various levels of government worked together to quickly develop a contact tracing operation, creating a web of people, including many hospital employees, who might have been exposed to the patients.
“The learning curve was so steep,” Rubin said. “Learning about the virus, but also learning how to do the surveillance and investigations … and how to document this in the best way, knowing this is on a scale that none of us had ever seen before.”
Both physicians recalled being surprised by how little the virus seemed to spread beyond the initial transmission from wife to husband, who had prolonged proximity from eating together, sleeping in the same bed and frequent face-to-face interaction.
“We didn’t see widespread transmission or a large number of secondary cases from this first case,” Joshi said. “I’ve always been sort of struck by that.”
About 350 contacts of both the husband and wife were actively monitored for symptoms, including 195 health care personnel and 152 contacts in the community, according to The Lancet article. Of the monitored contacts, 43 developed coronavirus-like symptoms within 14 days of exposure and were tested for the virus, along with a sample 32 asymptomatic health care workers who had some level of exposure.
But all 75 had tested negative for COVID-19, according to the article.
“The severity of illness, the extent of viral shedding, and timing of exposures to a symptomatic patient might all have contributed to the limited transmission described here,” said the article in The Lancet.
“Infection control measures within the hospital setting and an aggressive public health response might also have prevented further exposures.”
Nurse Monica Gomez recalled feeling fearful when she learned she’d be caring for the first confirmed coronavirus case in the state.
“I was scared for my life, because this was something unknown, it was a virus we had little research about,” said Gomez, who works in a medical-surgical unit at St. Alexius. “It was shocking to think it was in the United States. It was here, it was real. And I’m actually taking care of a COVID patient.”
To minimize exposure, the hospital had as few staff members as possible enter the room. Gomez recalled often communicating with the patient using an iPad translator, to help overcome a language barrier.
Under full personal protective equipment, the nurse had to keep visits to under 30 minutes, trying to cluster care as much as possible while balancing the patient’s medical and emotional needs.
Get her vitals. Do an assessment. Give any medication needed. Think of anything the patient might need, ice water, tea, fresh linens, to avoid extra trips, which would increase contact and waste protective equipment.
“Sometimes on the floor I’d think to myself. ‘I can’t even imagine how this patient’s handling this whole situation, lonely, not having their family come to visit them,'” Gomez said. “I think one thing I learned is that even a ‘good morning’ or making them smile can make a difference.”
Jaime Zalewski, infection preventionist, recalled waving to the patient from outside her room.
“You could see that she was scared,” Zalewski said. “If I were in her shoes, I’d be very scared too. They’re doing all these different tests, you’re sitting in a room by yourself. I was worried for her, for her well-being.”
The couple gave urine and stool samples for analysis. Blood was taken for serology testing. The wife and husband were also retested for the coronavirus every few days, back when uncomfortable nasopharyngeal swab tests, often dubbed the brain biopsy, were the only kind available.
Health officials said results took a while, because the CDC lab was the only facility processing them. The Illinois Department of Public Health became the first state in the nation to begin testing for the coronavirus in February, first at its Chicago lab and later at labs in Carbondale and Springfield.
“I’m sure she probably felt like a guinea pig,” Zalewski said. “And in some ways probably she was, because we just didn’t know. And that information we received has really helped shape not only our protocols, how we’re handling this emerging pathogen, but how our nation is handling the emerging pathogen.”
Condition reports for both patients were good throughout their hospitalization. Zalewski said the wife might not have even been admitted if she’d been infected with COVID-19 now.
The wife and husband were discharged to home isolation in early February, with daily monitoring by public health officials.
“They were happy they were able to go home together, that they were healthy going home,” Zalewski said.
But she described their departure as almost a covert operation. The wife and husband gave hospital staff permission to sanitize the inside of their car and then move it to secret location, to try and protect their privacy and avoid media attention as they left.
“They were scared to leave the hospital,” she said. “Scared of what could have potentially happened at their house, if people knew when they left. Was there going to be any backlash?”
They were cleared to leave their home in mid-February. Public health officials said they checked in with the couple last month, and both were still in good health.
Gomez and Zalewski said they’ve cared for many more COVID-19 patients as the pandemic continues, often applying what they learned from those first two cases. Illinois has had more than 250,000 positive cases so far, and more than 8,000 deaths, according to state health department statistics.
St. Alexius began celebrating COVID-19 recoveries by planting a flower-patterned pinwheel in front of the hospital for every coronavirus patient discharged.
While the tradition began after the wife and husband went home, Zalewski said staff made sure to include two pinwheels in honor of the first woman and man in Illinois to test positive and beat the virus.
“There’s definitely two flowers for those patients,” she said.
___
Distributed by Tribune Content Agency, LLC.