By Kristen V. Brown
Bloomberg News
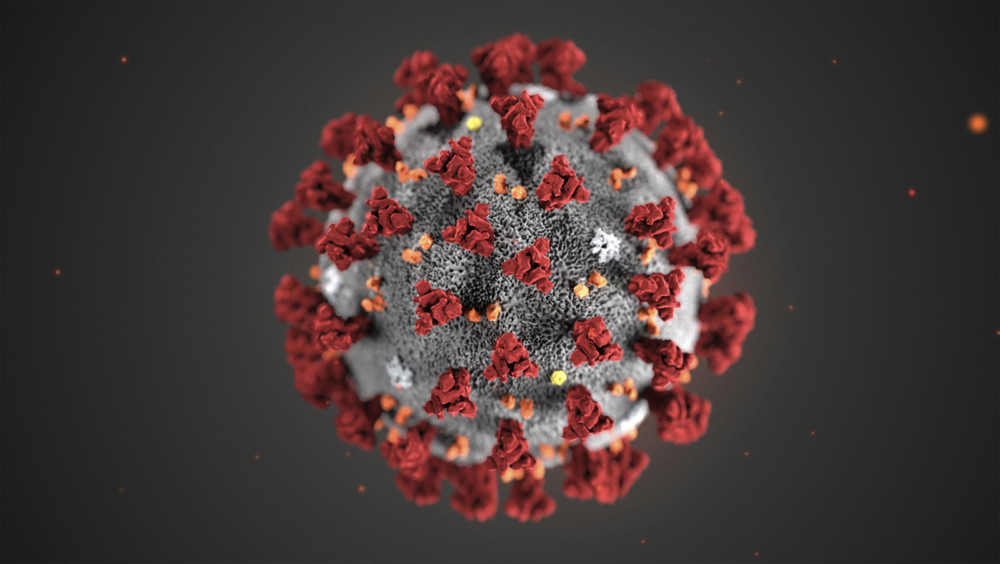
WWR Article Summary (tl;dr) Several ambitious antibody-test efforts are underway. These tests can indicate if a person has already been exposed to the virus and whether they have a level of immunity.
Bloomberg
As the U.S. begins to consider letting people go back to work and lifting social distancing rules, a new debate over testing is emerging. Researchers are racing to back-fill the gaping holes left by shortfalls in diagnostic tests for currently infected patients, with newly developed tests that can indicate if a person had COVID-19 previously.
These tests, which measure antibodies in the blood and are being used in studies across the U.S. and the rest of the world, are crucial to understanding COVID-19 and the virus that causes it. As they’re rolled out, they can tell researchers and government leaders not just how many people are sick but also how many have encountered the virus at all. That, in turn, may at last give a firmer idea of how deadly the virus is and how many people potentially have some level of immunity.
“We can’t see the virus. We can track it, its footprints in people. This is our best way to do that,” said Eric Topol, director of the Scripps Research Translational Institute. “We need to use this in conjunction with other means to try to restore some relative normalcy.”
Several studies already are underway. So far, early research suggests there are significant numbers of people who contract COVID-19 and don’t show symptoms. But there aren’t nearly enough of them to create widespread “herd immunity” that would build a societywide wall against infection and cause the virus to die out.
“We’re not anywhere near herd immunity,” Topol said. “An order of magnitude away, at the least.”
The tests search for antibodies, the immune system’s often long-lasting response to an infection, in the blood, instead of testing for the virus itself. The tests are typically conducted with drops of blood from a finger or a draw from a vein.
But, like the diagnostic tests that use a nose or throat swab to check currently infected patients, the blood antibody tests are proving to be a complex endeavor hamstrung by many of the same issues, as well as new ones.
A Stanford University study published online Friday prior to peer review concluded that more than twice as many people were infected with COVID-19 than current counts suggest, a number that would indicate it is both more widespread and less deadly than previously understood. This would mean Santa Clara County in California, which has had more than 1,800 positive cases, identified only 1 out of every 50 to 85 people who actually have COVID-19.
The study quickly drew criticism from experts.
It used Facebook ads to seek volunteers, who experts said may be more likely to have interest in such a test because they had symptoms, compared with a random sample of the population. Some also questioned the accuracy of the test itself.
“They assumed really, really high specificity,” Natalie Dean, a University of Florida biostatistician, said, using the term that indicates the rate at which false positives occur. “But the reality is that we don’t really know. They didn’t account for the uncertainty in that.”
Dean said weighting the results to better represent demographics of people who did not volunteer for the study also appeared to make it seem like more were infected.
“The results change a lot depending on what assumptions you put in,” Dean said. “I think there is value in getting an answer very quickly, even if it’s not exactly right. As long as it kind of gets us in a ballpark.”
The authors acknowledged in the paper there are issues with test accuracy, as well as other limitations of the study.
“No study, no matter how well done, will be able to give the definitive answer alone,” said John Ioannidis, a professor of medicine and epidemiology at Stanford who was involved in the study. “But at last we have data, real data, because until now we have mostly relied on speculation.”
In Los Angeles County, a collaborative study between the Department of Public Health and the University of Southern California estimated that about 4.1% of the county’s adult population has antibodies to the virus, or between 2.8% to 5.6% when accounting for potential errors. That estimate, researchers said, is 28 to 55 times higher than the 7,994 confirmed cases at the time of the study. Researchers conducted a rapid antibody test on a representative sample of the county population at six drive-through sites.
Both California numbers show a far higher rate of infection than some other, similar efforts. In China, Wuhan’s Zhongnan Hospital, for example, found that among 3,600 of its employees, a group particularly at risk of catching the virus, 2.4% had developed antibodies, doctors there said in a news conference earlier this month.
Other, similar studies have produced far different rates, adding to the ongoing debate about the virus’s spread. A much smaller one in the Boston suburb of Chelsea found that of 200 randomly sampled residents where were stopped on the street and asked to give some drops of blood, 64 had antibodies. The study was conducted by physicians at Massachusetts General Hospital.
John Iafrate, a pathologist at Harvard University and the study’s principal investigator, said the high numbers may be caused by high levels of community spread in Chelsea’s dense living conditions, as well as socioeconomic challenges.
“The good news is most people have mild disease,” he said. “We don’t know at this point what% of these antibody-positive individuals are still carrying virus, but a fair estimate is likely 30-50%.”
The Centers for Disease Control and Prevention has estimated that 25% of people may be asymptomatic for the disease. The U.S. has confirmed more than 805,000 known cases of COVID-19, but that number is widely thought to be an under-count.
Lacking any authoritative study, several ambitious antibody-test efforts have recently begun. The U.S. National Institutes of Health announced it would test 10,000 healthy volunteers for the presence of antibodies. New York, the state hardest-hit by the virus, has approved an antibody test that it is moving quickly to scale up.
Several manufacturers have announced tests that could not only assess the disease’s spread but also identify potentially immune people who could go back to work, reopen schools or help prove whether future vaccines are working. Abbott Laboratories has said it will ship 4 million of its new antibody tests this month, with the goal of manufacturing 20 million a month by June.
Because of the desire to get more of the tests to market, the U.S. Food and Drug Administration has relaxed the usual assessment criteria for them. But not all of the tests have performed perfectly. The FDA has allowed dozens of tests to come to market without the usual vetting. There is evidence many underperform: The agency issued a warning last week urging awareness that not all such tests have been approved and that health care providers should “be aware of their limitations.” Just four tests have received official emergency authorization from the agency.
“The technology behind antibody tests is fundamentally distinct and generally harder to get right,” Anna Petherick, a public policy expert at the University of Oxford wrote recently in the journal The Lancet.
Developing antibody tests requires more knowledge of a specific virus’s structure than a diagnostic test does. To make the tests, researchers produce sections of proteins from the virus that the human immune system responds to. Different tests check for different antibodies, but these antibodies can vary from person to person. And not all of them are the type of antibodies that indicate potential immunity. There also are concerns that the tests could pick up antibodies from other strains of coronavirus that cause different, milder illnesses, like a common cold. And even with the right test, findings can vary significantly from region to region.
“Each population at each moment in time is different,” said Marc Lipsitch, a Harvard University epidemiologist who critiqued the Stanford study. “And it’s really hard to compare across populations.”
But, said Lipsitch, even imperfect studies add to our knowledge of a virus that until a few months ago was entirely unknown. The picture may be fuzzy, but it is beginning to come into focus.
“We have some sense that maybe the prevalence of infection is a lot larger than we thought it was,” he said. “This is now an estimate of how much larger. But that estimate is quite uncertain.”
___
Distributed by Tribune Content Agency, LLC.